
How Harm Reduction Can Help Combat the Overdose Crisis
Harm reduction is an essential part of recovery. It can save lives, it can protect communities and if ignored, it can make an epidemic even worse.

Sean Paul Mahoney is the author of the new collection of essays Now That You’ve Stopped Dying and the co-host of the LGBTQ recovery podcast Queer Mental Condition. He also works as a recovery mentor and peer support specialist in Portland, Oregon.

Harm reduction is an essential part of recovery. It can save lives, it can protect communities and if ignored, it can make an epidemic even worse.

Alcohol use within the LGBTQ+ community is a serious problem. Sean Paul Mahoney is here to educate us on the issue and how to overcome the sponsored pride.

When it comes to meth, there’s no MAT, no funding, and little hope For being in the middle of an opioid epidemic, we sure did

Here are some important tips and talking points that can make a real difference when you talk about harm reduction and substance use. When I
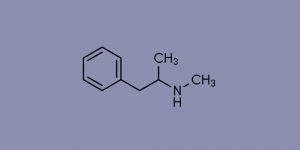
Withdrawal from meth can be uncomfortable, but there are tools to help you get through it, and freedom waiting on the other side. When you’re
For most of us, the road to recovery is filled with a whole bunch of “shoulda, woulda, coulda” thoughts. “Should’ve stopped drinking sooner,” and “Would’ve

In the blah days of January, way after whatever holiday sparkle we were able to muster up has gone, what are we left with? Personally, as a man in long-term recovery, I find myself incredibly grateful at the end of the holidays for the gift of boundaries.

Shaun Paul Mahoney is here to talk about the hit Netflix show, The Queens Gambit, and what it gets right about addiction.

Sean Paul Mahoney wrote a great blog about the radical act of gratitude and how it helped it in his recovery.

Alcohol consumption during COVID is on the rise. Sean Paul Mahoney is here to talk about how to catch the signs of if you should quit drinking alcohol.

Sean Paul Mahoney talks about how they did a digital detox. They give great tips for how to ease into using less social media or how to abstain completely.
Somewhere along day fortysomething of quarantine, I’d had it. Sean Paul Mahoney is here to tell you about staying in the moment even when the moment sucks.

During the pandemic, we are all dealing with our own crisis inside of the crisis. Like boredom, jealousy, etc.

If you were only to look online and never meet real sober folks you might think that we’re all nice, straight white people. Yet despite

“We’re Really Worried About You”: When Loved Ones have THE TALK About Your Drinking and Using. There are certain conversations burned into your mind that

Having recently celebrated 11 years sober, it occurred to me that drinking and using has changed since I stopped. Not changed in a way like,

Suboxone (buprenorphine/naloxone) is indicated for the treatment of opioid dependence in adults. Suboxone should not be taken by individuals who have been shown to be hypersensitive to buprenorphine or naloxone as serious adverse reactions, including anaphylactic shock, have been reported. Taking Suboxone (buprenorphine/naloxone) with other opioid medicines, benzodiazepines, alcohol, or other central nervous system depressants can cause breathing problems that can lead to coma and death. Other side effects may include headaches, nausea, vomiting, constipation, insomnia, pain, increased sweating, sleepiness, dizziness, coordination problems, physical dependence or abuse, and liver problems. For more information about Suboxone (buprenorphine/naloxone) see Suboxone.com, the full Prescribing Information, and Medication Guide, or talk to your healthcare provider. You are encouraged to report negative side effects of drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
All clinical and medical services are provided by licensed physicians and clinicians who are practicing as employees or contractors of independently owned and operated professional medical practices that are owned by licensed physicians. These medical practices include Workit Health (MI), PLLC, Workit Health (CA), P.C., Workit Health (NJ), LLC, Workit Health (OH), LLC, and any other Workit Health professional entity that is established in the future.
Arizona
9700 N. 91st. St.
Ste A-115
Scottsdale, AZ 85258
fax (HIPAA): (833) 664-5441
Florida
4730 North Habana Ave
Ste 206
Tampa, FL 33614
fax (HIPAA): (813) 200-2822
Illinois
1280 Iroquois Ave
Ste 402
Naperville, IL 60563
fax (HIPAA): (855) 716-4494
Michigan
3300 Washtenaw Ave
Ste 280
Ann Arbor, MI 48104
fax (HIPAA): (855) 716-4494
Montana
415 N Higgins Ave
Ste 6
Missoula, MT 59802
fax (HIPAA): (855) 716-4494
New Jersey
5 Greentree Center
Ste 117
Marlton, NJ 08053
fax (HIPAA): (609) 855-5027
New Mexico
5901 Indian School Road, NE
Ste 212
Albuquerque, NM 87110
fax (HIPAA): (855) 716-4494
Ohio
6855 Spring Valley Dr
Ste 110
Holland, OH 43528
fax (HIPAA): (513) 823-3247
Oklahoma
1010 24th Ave NW
Suite 100
Norman, OK 73069
fax (HIPAA): (855) 716-4494
Texas
8229 Shoal Creek Blvd
Ste 105
Austin, TX 78757
fax (HIPAA): (737) 738-5046
Clinic locations
Arizona
9700 N. 91st. St.
Ste A-115
Scottsdale, AZ 85258
fax (HIPAA): (833) 664-5441
Florida
600 Heritage Dr.
Ste 210, #17
Jupiter, FL 33458
fax (HIPAA): (813) 200-2822
Illinois
1280 Iroquois Ave
Ste 402
Naperville, IL 60563
fax (HIPAA): (855) 716-4494
Michigan
3300 Washtenaw Ave
Ste 280
Ann Arbor, MI 48104
fax (HIPAA): (855) 716-4494
Montana
415 N Higgins Ave
Ste 6
Missoula, MT 59802
fax (HIPAA): (855) 716-4494
New Jersey
5 Greentree Center
Ste 117
Marlton, NJ 08053
fax (HIPAA): (609) 855-5027
New Mexico
5901 Indian School Road, NE
Ste 212
Albuquerque, NM 87110
fax (HIPAA): (855) 716-4494
Ohio
6855 Spring Valley Dr
Ste 110
Holland, OH 43528
fax (HIPAA): (513) 823-3247
Texas
5373 W Alabama St
Ste 204
Houston, TX 77056
fax (HIPAA): (737) 738-5046
Oklahoma
1010 24th Ave NW
Suite 100
Norman, OK 73069
fax (HIPAA): (855) 716-4494
This site uses cookies to improve your experience. By using this site, you consent to our use of cookies.