First Responders: Addiction and Mental Health
First responders carry the weight of so many lives, emergencies, and disasters. Despite their skill and training, first responders are still human, and the pressures of their work make them susceptible to addiction and mental health disorders.
First Responders: Addiction and Mental Health

First responders carry the weight of so many lives, emergencies, and disasters. Despite their skill and training, first responders are still human, and the pressures of their work make them susceptible to addiction and mental health disorders.
First responders face unique challenges in treating their mental health and addiction.
During an emergency, first responders are on call and on the scene to provide much-needed assistance. Police, firefighters, emergency medical services, and other rescue workers persevere through pain, danger, and stress to protect others from harm.
While officers exhibit amazing levels of dedication and sacrifice, they are still human. As humans, constant exposure to the physical and mental health challenges in this line of work places officers at high risk of developing mental health conditions. An estimated 30% of responders live with disorders like depression and PTSD.
Many first responders turn to alcohol and other addictive substances to cope with the strain. One study reported that 58% of career firefighters and 40% of volunteer firefighters drank heavily on their days off.
Dealing with mental health concerns and substance use disorders as a first responder can be challenging for many reasons, from the culture of silence to the stigma surrounding an officer seeking help rather than giving it.
First responders struggling with these issues need to know that they are not weak and they are not alone. Help is available.
Substance use among police officers
Police officers regularly intervene in dangerous scenarios and witness personal struggles. As an expected part of their roles, they relay bad news and cope with the loss of their colleagues.
Law enforcement often demands long and irregular hours. Some of the other known struggles police officers face include working shifts over holidays, work-related injuries, and dealing with poor public perception of force by their local communities and neighbors. At work, they may also encounter a stoic culture that expects officers to “tough it out,” managing all of these stresses without voicing complaints.
To cope, many officers turn to alcohol or drugs. A 2011 study recorded a 7.8% incidence of lifetime alcohol abuse in a police unit. Around 11% of male and 15% of female officers were viewed as at risk of alcohol dependence. This is exacerbated by the hard-drinking culture in many precincts. Officers are also at high risk of drug use. Many begin by taking stimulants to help them stay awake through long shifts or opioids to handle physical (often chronic) pain, and find themselves with a substance use problem they never expected.
Police officers’ concerns about seeking addiction treatment
Many law enforcement officers struggle with alcohol use disorder and substance use disorder alone, feeling wary of seeking treatment. Here are some of the concerns we’ve heard from police officers:
- Many officers are reluctant to trust doctors and health experts, especially if they aren’t confident that they already treat members of law enforcement.
- Police officers are subject to fit-for-duty evaluations. Seeking help to deal with mental health or substance use could affect their performance and threaten their job security.
- Police officers may be restricted from taking part in some kinds of treatment. For example, in many areas, police officers are barred from using methadone or buprenorphine to treat opioid use disorder. Knowing that certain avenues of treatment are off-limits to them, some officers prefer not to seek treatment at all.
- Substance use disorders are heavily stigmatized in general. It can be even more looked down upon in a profession that is responsible for arresting people who sell and possess illicit drugs and who drive under the influence of alcohol and other substances. The fear of anyone discovering their use can keep officers from looking for help.
These concerns are understandable and serious, but they should not keep a police officer trapped in a cycle of substance use. Doctors who treat addiction and substance use disorder are discreet and bound by HIPAA. And while certain prescriptions must be reported to a state’s Prescription Drug Monitoring Program, there are other treatment options available.
Substance use among firefighters
Firefighters routinely deal with the devastation of fire, provide support to accident victims, and assist with rescue missions caused by natural disasters. For many firefighters, alcohol and other substances can seem like a necessary form of self-medication that allows them to weather the difficulties of work-life.
This job description can often come with its fair share of trauma, which can cause insomnia, nightmares, anxiety, PTSD, and other mental health disorders. Many firefighters use alcohol both as a way to cope with these difficulties and to bond with their fellows in the fire brigade.
Firefighters are also prone to work-related injuries and chronic pain, which may lead to dependence on pain medications.
Fire fighters’ concerns about seeking addiction treatment
Many firefighters struggle with substance use or mental health but put off getting treatment. Here are some of the concerns we’ve heard from firefighters:
- Firefighters may feel a lack of trust that health experts will understand firefighter culture.
- Volunteer firefighters may lack access to effective addiction treatment that can help them overcome substance abuse. In contrast, career firefighters may have access to treatment through organizational insurance or employee assistance programs but hesitate to use them out of fear that their chief or brigade will know.
- Firefighters live and work with their peers. This proximity may cause a firefighter to resist scenarios that cause them to stand out as different, e.g, seeking help for substance abuse.
- Some firefighters consider it a show of weakness to seek help for a dependency.
While distrust, lack of access, and social stigma are barriers to getting treatment, there are more treatment options now than there ever have been before, many of which can overcome these obstacles. For those who don’t have commercial insurance, many addiction treatment providers accept payment options like Medicaid and self-pay. Telemedicine has also opened up flexible new avenues of treatment that can be very discreet, as one can attend appointments and complete therapy from anywhere.
Substance use among Emergency Medical Technicians
EMTs and paramedics provide urgent care to accident victims and those in need of pressing medical attention. In their daily roles, these responders come in contact with car wrecks, drug overdoses, stabbings, and more.
EMTs take on considerable trauma when carrying out their duties, and many develop mental health issues as a result. This can encourage the use of unhealthy coping mechanisms, like drinking and drug use.
EMTs’ and paramedics’ concerns about seeking addiction treatment
Many EMTs struggle with substance use or mental health but put off getting treatment. Here are some of the concerns we’ve heard from EMTs and paramedics:
- Many EMTs identify with their role as the strong care-provider and fear appearing weak by seeking expert help.
- EMTs and paramedics may worry about a breach of confidentiality should they seek outside help, including fear of professional repercussions.
- With round-the-clock demands, EMTs may not have the time to spare for treatment at rehabs.
- In many parts of the country, EMTs are underpaid and may have difficulty affording traditional treatment.
These concerns can be serious, but they should not keep EMTs and paramedics from getting the help they deserve. Health care providers who treat substance use disorder follow HIPAA guidelines to protect privacy. And there are treatment options that are more flexible and affordable than traditional rehab.
Police Officers
Police officers regularly intervene in dangerous scenarios and witness personal struggles. As an expected part of their roles, they relay bad news and cope with the loss of their colleagues.
Law enforcement often demands long and irregular hours. Some of the other known struggles police officers face include working shifts over holidays, work-related injuries, and dealing with poor public perception of force by their local communities and neighbors. At work, they may also encounter a stoic culture that expects officers to “tough it out,” managing all of these stresses without voicing complaints.
To cope, many officers turn to alcohol or drugs. A 2011 study recorded a 7.8% incidence of lifetime alcohol abuse in a police unit. Around 11% of male and 15% of female officers were viewed as at risk of alcohol dependence. This is exacerbated by the hard-drinking culture in many precincts. Officers are also at high risk of drug use. Many begin by taking stimulants to help them stay awake through long shifts or opioids to handle physical (often chronic) pain, and find themselves with a substance use problem they never expected.
Police officers’ concerns about seeking addiction treatment
Many law enforcement officers struggle with alcohol use disorder and substance use disorder alone, feeling wary of seeking treatment. Here are some of the concerns we’ve heard from police officers:
- Many officers are reluctant to trust doctors and health experts, especially if they aren’t confident that they already treat members of law enforcement.
- Police officers are subject to fit-for-duty evaluations. Seeking help to deal with mental health or substance use could affect their performance and threaten their job security.
- Police officers may be restricted from taking part in some kinds of treatment. For example, in many areas, police officers are barred from using methadone or buprenorphine to treat opioid use disorder. Knowing that certain avenues of treatment are off-limits to them, some officers prefer not to seek treatment at all.
- Substance use disorders are heavily stigmatized in general. It can be even more looked down upon in a profession that is responsible for arresting people who sell and possess illicit drugs and who drive under the influence of alcohol and other substances. The fear of anyone discovering their use can keep officers from looking for help.
These concerns are understandable and serious, but they should not keep a police officer trapped in a cycle of substance use. Doctors who treat addiction and substance use disorder are discreet and bound by HIPAA. And while certain prescriptions must be reported to a state’s Prescription Drug Monitoring Program, there are other treatment options available.
Fire Fighters
Firefighters routinely deal with the devastation of fire, provide support to accident victims, and assist with rescue missions caused by natural disasters. For many firefighters, alcohol and other substances can seem like a necessary form of self-medication that allows them to weather the difficulties of work-life.
This job description can often come with its fair share of trauma, which can cause insomnia, nightmares, anxiety, PTSD, and other mental health disorders. Many firefighters use alcohol both as a way to cope with these difficulties and to bond with their fellows in the fire brigade.
Firefighters are also prone to work-related injuries and chronic pain, which may lead to dependence on pain medications.
Many firefighters struggle with substance use or mental health but put off getting treatment. Here are some of the concerns we’ve heard from firefighters:
- Firefighters may feel a lack of trust that health experts will understand firefighter culture.
- Volunteer firefighters may lack access to effective addiction treatment that can help them overcome substance abuse. In contrast, career firefighters may have access to treatment through organizational insurance or employee assistance programs but hesitate to use them out of fear that their chief or brigade will know.
- Firefighters live and work with their peers. This proximity may cause a firefighter to resist scenarios that cause them to stand out as different, e.g, seeking help for substance abuse.
- Some firefighters consider it a show of weakness to seek help for a dependency.
While distrust, lack of access, and social stigma are barriers to getting treatment, there are more treatment options now than there ever have been before, many of which can overcome these obstacles. For those who don’t have commercial insurance, many addiction treatment providers accept payment options like Medicaid and self-pay. Telemedicine has also opened up flexible new avenues of treatment that can be very discreet, as one can attend appointments and complete therapy from anywhere.
Emergency Medical Technicians
EMTs and paramedics provide urgent care to accident victims and those in need of pressing medical attention. In their daily roles, these responders come in contact with car wrecks, drug overdoses, stabbings, and more.
EMTs take on considerable trauma when carrying out their duties, and many develop mental health issues as a result. This can encourage the use of unhealthy coping mechanisms, like drinking and drug use.
Many EMTs struggle with substance use or mental health but put off getting treatment. Here are some of the concerns we’ve heard from EMTs and paramedics:
- Many EMTs identify with their role as the strong care-provider and fear appearing weak by seeking expert help.
- EMTs and paramedics may worry about a breach of confidentiality should they seek outside help, including fear of professional repercussions.
- With round-the-clock demands, EMTs may not have the time to spare for treatment at rehabs.
- In many parts of the country, EMTs are underpaid and may have difficulty affording traditional treatment.
These concerns can be serious, but they should not keep EMTs and paramedics from getting the help they deserve. Health care providers who treat substance use disorder follow HIPAA guidelines to protect privacy. And there are treatment options that are more flexible and affordable than traditional rehab.

Signs of Addiction in First Responders
Drinking and drug use can often be casual and socially acceptable, which can make it difficult to tell when they are becoming a problem. But there are some signs of addiction to look out for. Primarily, these signs are changes in behavior:
- Isolation from others
- Difficulty carrying out daily responsibilities
- Mood or personality changes
- Spending large sums of money
- Asking for financial assistance
- Making excuses to rationalize or cover up how much they’re drinking or using
In general, when drinking or drug use has negative life consequences, it’s a red flag.
When someone is hiding their substance use, there can be observable signs, which include:
- Dilated pupils
- Increase or decrease in weight
- Tremors or shakiness
- Change in skin tone
- Compromised decision making
- Poor coordination
- Jumpiness
- Increased or reduced energy levels
- Changes in sleep patterns
- Changes in appetite
- Slurred or unclear speech
Getting help for addiction
It’s estimated that only one in ten people who need treatment for addiction receive it. First responders are often among the majority who struggle alone, whether out of fear of professional consequences, lack of access to treatment, difficult work schedules, or peer pressure that normalizes substance use while dismissing help. Despite these concerns, first responders deserve support to get their lives back. And taking care of themselves will make them better equipped to protect and rescue others.
Treatment can offer support that will help stabilize addiction recovery and care for the other mental health concerns that might be tied to substance use. While many first responders do not feel able to go away to an in-person rehab for thirty or sixty days, the rise in telemedicine has made it possible to receive effective, science-backed addiction treatment via phone or computer. Workit Health’s app is secure and discreet, and offers both clinical treatment and behavioral health support from the privacy of home.

Start your recovery
No waiting rooms, no judgment, just easy streamlined virtual recovery care
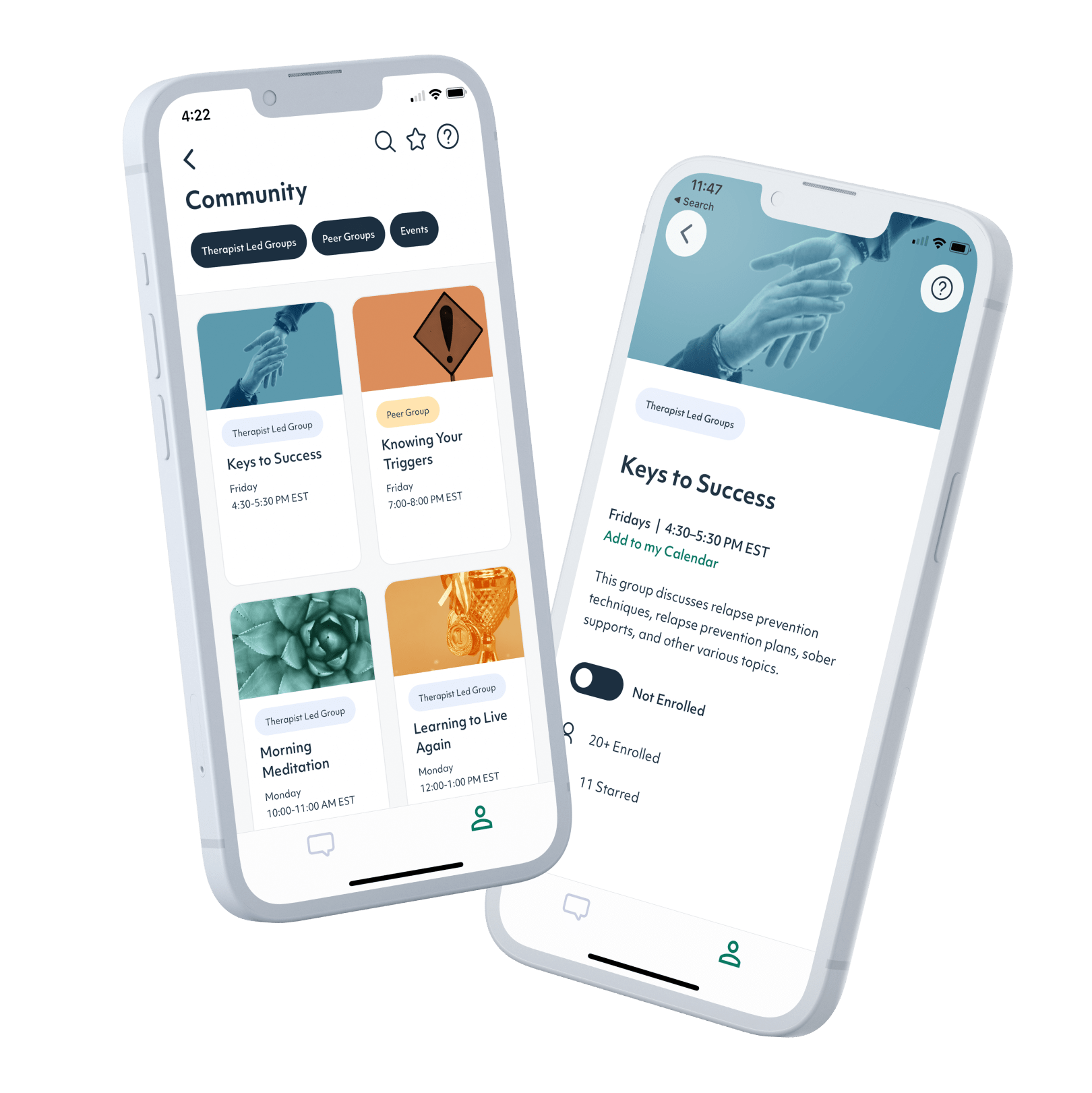
1. Sign up
It only takes a few minutes. Download our app and answer a few questions about your treatment goals, then schedule your first appointment.
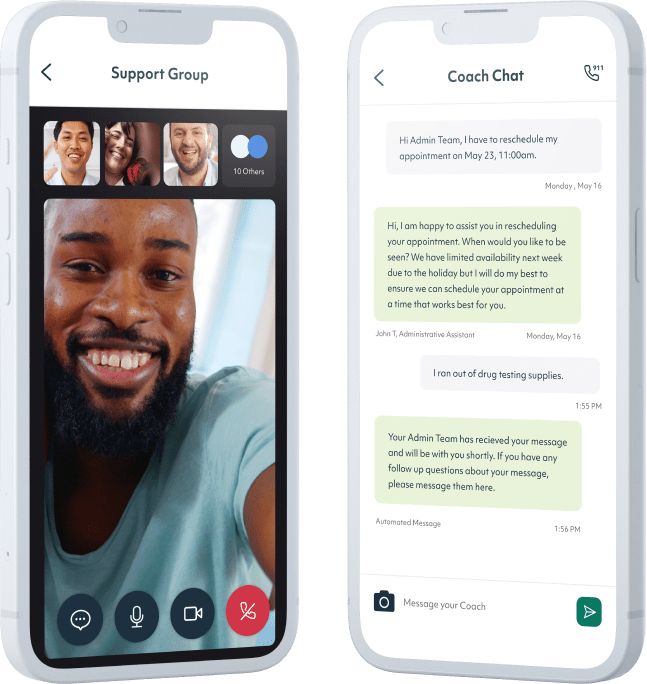
2. Meet with a provider
Meet with a licensed provider via a secure video appointment to set your recovery goals and establish your treatment plan.
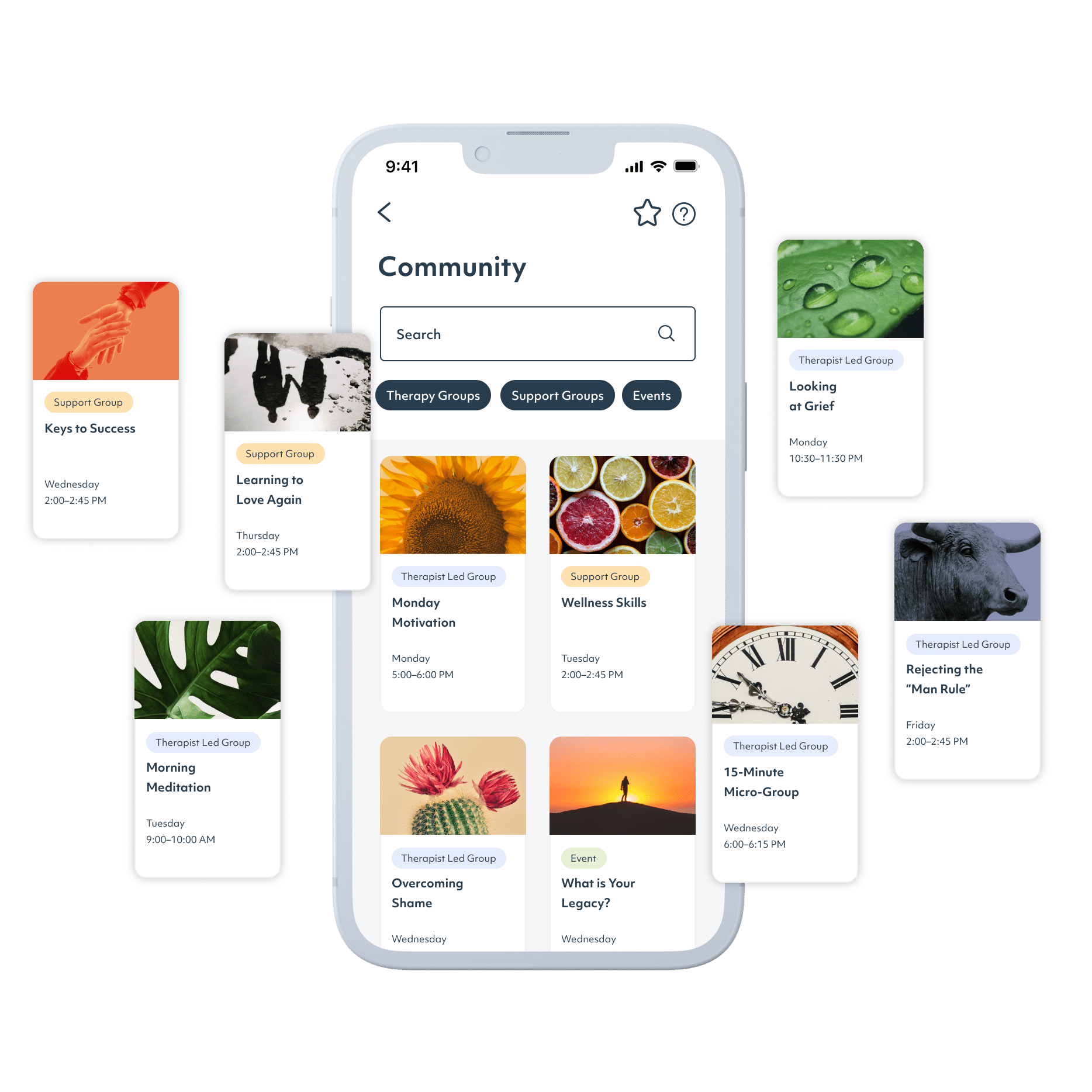
3. Get ongoing support
Shared Follow-up Appointments, recovery groups, and online community provide support and help you build skills to navigate life sober.
No waiting rooms, no judgment, just easy streamlined virtual recovery care
Trusted by major insurance providers
Find your state
Medication-assisted treatment
Citations
1. First Responders: Behavioral Health Concerns, Emergency Response, and Trauma. Substance Abuse and Mental Health Services Administration (SAMHSA). https://www.samhsa.gov/sites/default/files/dtac/supplementalresearchbulletin-firstresponders-may2018.pdf. May 2018.
2. C. K. Haddock, S. A. Jahnke, W. S. C. Poston, N. Jitnarin, C. M. Kaipust, B. Tuley, & M. L. Hyder. (2012). Alcohol use among firefighters in the Central United States. Occupational Medicine, 62 (8), 661–664. https://doi.org/10.1093/occmed/kqs162
3. Ballenger, J. F., Best, S. R., Metzler, T. J., Wasserman, D. A., Mohr, D. C., Liberman, A., Delucchi, K., Weiss, D. S., Fagan, J. A., Waldrop, A. E., & Marmar, C. R. (2011). Patterns and predictors of alcohol use in male and female urban police officers. The American journal on addictions, 20(1), 21–29. https://doi.org/10.1111/j.1521-0391.2010.00092.x
4. Vollmer, H. C., & Domma, J. (2020). Différence de réussite au traitement hospitalier entre dépendants à l’alcool et dépendants aux drogues illicites : une étude de reproductibilité [Differences in the success rates of inpatient therapy for alcohol and illegal drug abusers. A Replication Study]. L’Encephale, 46(2), 102–109. https://doi.org/10.1016/j.encep.2019.09.008





